
If you have diabetes, reduce your risk of getting diabetic retinopathy by doing the following: However, regular eye exams, good control of your blood sugar and blood pressure, and early intervention for vision problems can help prevent severe vision loss. You can't always prevent diabetic retinopathy.

Diabetic retinopathy, macular edema, glaucoma or a combination of these conditions can lead to complete vision loss, especially if the conditions are poorly managed. This pressure can damage the nerve that carries images from your eye to your brain (optic nerve). New blood vessels can grow in the front part of your eye (iris) and interfere with the normal flow of fluid out of the eye, causing pressure in the eye to build. This can cause spots floating in your vision, flashes of light or severe vision loss. The abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye. Unless your retina is damaged, your vision will likely return to its previous clarity. The blood often clears from the eye within a few weeks or months. Vitreous hemorrhage by itself usually doesn't cause permanent vision loss. In more-severe cases, blood can fill the vitreous cavity and completely block your vision. If the amount of bleeding is small, you might see only a few dark spots (floaters). The new blood vessels may bleed into the clear, jellylike substance that fills the center of your eye. Complications can lead to serious vision problems: This buildup can damage the nerve that carries images from your eye to your brain (optic nerve), resulting in glaucoma.ĭiabetic retinopathy involves the growth of abnormal blood vessels in the retina. If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure can build in the eyeball. These new blood vessels are fragile and can leak into the clear, jellylike substance that fills the center of your eye (vitreous).Įventually, scar tissue from the growth of new blood vessels can cause the retina to detach from the back of your eye. In this type, damaged blood vessels close off, causing the growth of new, abnormal blood vessels in the retina. Diabetic retinopathy can progress to this more severe type, known as proliferative diabetic retinopathy. If macular edema decreases vision, treatment is required to prevent permanent vision loss.Īdvanced diabetic retinopathy. Sometimes retinal blood vessel damage leads to a buildup of fluid (edema) in the center portion (macula) of the retina. NPDR can progress from mild to severe as more blood vessels become blocked. Larger retinal vessels can begin to dilate and become irregular in diameter as well.

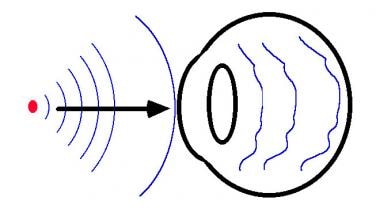
Tiny bulges protrude from the walls of the smaller vessels, sometimes leaking fluid and blood into the retina. When you have nonproliferative diabetic retinopathy (NPDR), the walls of the blood vessels in your retina weaken. In this more common form - called nonproliferative diabetic retinopathy (NPDR) - new blood vessels aren't growing (proliferating). There are two types of diabetic retinopathy:Įarly diabetic retinopathy. But these new blood vessels don't develop properly and can leak easily. As a result, the eye attempts to grow new blood vessels. Over time, too much sugar in your blood can lead to the blockage of the tiny blood vessels that nourish the retina, cutting off its blood supply.


 0 kommentar(er)
0 kommentar(er)
